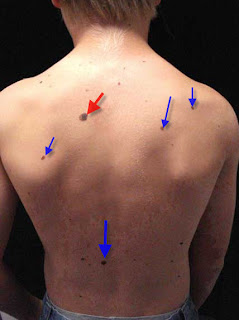
Abstract: 12 yo boy referred for evaluation of nevi
History: The boy's pediatrician referred him for evaluation of nevi. There is no pertinent family history since he is adopted. His mother feels the large lesion on the back has changed over the past year.
O/E: Healthy child. Type II skin. All nevi, except one, look similar. The "outlier lesion" measures 1 cm in diameter, has variations in color and a white area.
Clinical Photo(s):
Dermoscopic Image

Lab: N/A
Histopathology: N/A
Diagnosis or DDx: Probable Dysplastic Nevus Syndrome in a 12 yo boy.
Questions: What would you do here?
Reason(s) Presented: To discuss the concept of the "ugly duckling" (outlier lesions). Lesions which stand out as not belonging with the others a patient has deserve more attention and one should have a lower index of suspicion for biopsying.
Discussion: Dr. Riemann
Dysplastic melanocytic nevi (DMN) are a heterogenuous group of nevi with atypical clinical features, histopathologic abnormalities, or both.
The clinical features of DMN include asymmetry, varying sizes frequently larger than regular melanocytic nevi, irregular or ill-defined borders, some color variegation showing two to three shades of brown, pink, skin-colored, or red, and surface irregularities like "cobblestoning" or "fried-egg" appearance. Histopathologically, DMN can show lentiginous proliferation, elongated or bridged rete ridges, nests varying in size, nest located in papillary tips, a junctional component extending beyond the dermal component, and some degree of cytologic pleomorphism.
Several studies have shown that the risk of melanoma is directly related to the number of ordinary nevi and to the number of DMN as defined by the clinical criteria above.
Although the term "dysplastic nevus syndrome" lacks a stringent definition, it is ususally used to describe an autosomal dominant condition of increased number of ordinary and DMN. Affected individuals have an increased risk to develop melanoma and therefore, require regular skin checks. As these patients, by definition, can have many clinically atypical nevi, the challenging task for the clincian is to identify any lesions suspicious for melanoma.
The "outlier" concept describes a helpful rule of thumb to look for any DMN which appears to clearly stand out as being different from the average, baseline clinical appearance of the patient's other nevi. These "outlier lesions" should be carefully evaluated for removal. Lesions suspicious for melanoma should then be removed with a 2-5 mm margin when possible
.
References:
1. Grob JJ, Bonerandi JJ.
The 'ugly duckling' sign: identification of the common characteristics of nevi in an individual as a basis for melanoma screening. Arch Dermatol. 1998 Jan;134(1):103-4
2. Dixon AJ, Hall RS. Managing skin cancer--23 golden rules. Aust Fam Physician. 2005 Aug;34(8):669-71.
From their collective experience in Australia and the USA, dermasurgeons Anthony Dixon and Scott Hall have compiled a list of "golden rules" for general practitioners to help reduce errors and problems with skin cancer management. It is anticipated that these tips will provide a brief yet informative reference when faced with skin cancer management concerns in general practice.
This valuable refrence can be viewed as FULL TEXT HERE
3. Emedicine.com has a good chapter on Dysplastic Nevi.